
Understanding Leprosy and Available Treatments
As a pharmacist, one of the most important parts of my job is dispelling fear with facts. Few diseases carry as much historical stigma as leprosy, yet few are as misunderstood. In the modern medical world, leprosy—clinically known as Hansen’s Disease—is not a curse or a highly contagious plague. It is a chronic bacterial infection that is completely curable with the right medication.
This guide delves into the pathology of leprosy, how to recognize it, and most importantly, the specific pharmacological treatments that have transformed it from a lifelong sentence into a manageable, curable condition.
What is Leprosy (Hansen’s Disease)?
Leprosy is a chronic infectious disease caused by a slow-growing acid-fast bacterium called Mycobacterium leprae. It primarily affects the skin, the peripheral nerves, the mucosa of the upper respiratory tract, and the eyes.
It is crucial to understand that leprosy is not highly contagious. Approximately 95% of the human population has a natural immunity to the bacteria. For the remaining 5%, transmission occurs via droplets from the nose and mouth during close and frequent contact with untreated cases. It is not spread through casual contact like shaking hands or sitting next to someone on a bus.
The Incubation Period
One unique characteristic of M. leprae is its slow replication rate. The incubation period—the time from infection to the appearance of symptoms—is typically 5 years but can range from 1 year to as long as 20 years. This delay often makes it difficult to pinpoint exactly when or where a patient contracted the infection.
Recognizing the Symptoms: Early Detection is Key
From a pharmaceutical care perspective, early diagnosis is vital to preventing permanent nerve damage. The bacteria attack the Schwann cells (which insulate our nerves), leading to loss of sensation.
1. Cutaneous (Skin) Signs
The hallmark sign is a skin patch that looks different from the surrounding area. These patches may be:
- Hypopigmented (lighter than the surrounding skin) or reddish.
- Flat or raised.
- Crucial Test: These patches often lack sensation. If you prick the area with a pin or touch it with hot/cold objects, the patient may feel nothing.
2. Neural (Nerve) Signs
Because the bacteria target peripheral nerves, patients may experience:
- Numbness or tingling in the hands or feet.
- Thickened, painful, or tender nerves (often felt at the elbow or knee).
- Muscle weakness or paralysis (e.g., foot drop or inability to close the eye).
3. Advanced Symptoms (If Untreated)
Without antibiotic intervention, the damage progresses to:
- Tissue loss in fingers and toes (due to repeated injury in numb areas, not the bacteria “eating” the flesh).
- Blindness (due to corneal ulcers or lagophthalmos).
- Disfigurement of the nose (saddle nose deformity).
Classification for Treatment Purposes
Before dispensing medication, a clinician must classify the type of leprosy to determine the correct drug regimen. The World Health Organization (WHO) classifies leprosy based on the number of skin lesions:
- Paucibacillary (PB) Leprosy: 1 to 5 skin lesions. The skin smear test is negative for bacteria.
- Multibacillary (MB) Leprosy: More than 5 skin lesions. The skin smear is positive, or there is significant nerve involvement.
Pharmacological Treatment: Multi-Drug Therapy (MDT)
This is the most critical section for understanding the cure. Since 1981, the WHO has recommended Multi-Drug Therapy (MDT). Using a single antibiotic (monotherapy) is strictly avoided because M. leprae can easily develop resistance. MDT combines different mechanisms of action to ensure all bacteria are killed effectively.
As a pharmacist, I counsel patients on three primary antibiotics used in MDT:
1. Rifampicin (The Bactericidal Powerhouse)
- Role: Rifampicin is the most important drug in the regimen. It is highly bactericidal, meaning it actively kills the bacteria. A single dose can kill 99.9% of viable M. leprae organisms.
- Mechanism: It inhibits bacterial RNA synthesis.
- Patient Counseling:
- Urine Discoloration: I always warn patients that this drug will turn their urine, sweat, and tears a reddish-orange color. This is harmless but can be alarming if not expected.
- Administration: Typically taken once a month under supervision.
2. Dapsone (The Bacteriostatic Agent)
- Role: Dapsone stops the bacteria from multiplying (bacteriostatic). It has been used since the 1940s.
- Mechanism: It inhibits folate synthesis, which the bacteria need to survive.
- Patient Counseling:
- Daily Dosing: This is usually taken daily at home.
- Allergy Watch: We monitor for “Dapsone Syndrome” (fever, rash, and organ involvement), though rare. Patients with a G6PD deficiency must be monitored closely to prevent anemia.
3. Clofazimine (The Anti-Inflammatory Antibiotic)
- Role: Used primarily for MB leprosy, Clofazimine is both anti-bacterial and anti-inflammatory.
- Mechanism: It binds to the DNA of the bacteria.
- Patient Counseling:
- Skin Discoloration: This drug causes a brownish-black discoloration of the skin and conjunctiva. This is the most common reason for non-adherence. I reassure patients that this discoloration is reversible and will fade months after treatment ends.
- Gastrointestinal Issues: It can sometimes cause abdominal pain.
The Standard WHO Regimens
We dispense these drugs in “blister packs” (calendar packs) to improve adherence.
| Leprosy Type | Drugs Used | Duration | Notes |
| Paucibacillary (PB) | Rifampicin + Dapsone | 6 Months | Used for lower bacterial loads. |
| Multibacillary (MB) | Rifampicin + Clofazimine + Dapsone | 12 Months | Used for higher bacterial loads. |
Note: In some countries, the regimen may be extended based on national guidelines.
Managing Leprosy Reactions
Even while on treatment, or after treatment is finished, the immune system may react violently to the dead bacteria remaining in the body. These are called Leprosy Reactions. They are medical emergencies and must be treated immediately to prevent nerve damage.
- Type 1 Reaction (Reversal Reaction): Inflammation of existing skin patches and nerves.
- Treatment: Usually involves high-dose corticosteroids (like Prednisolone) to reduce swelling around the nerves.
- Type 2 Reaction (ENL – Erythema Nodosum Leprosum): Painful red nodules on the skin, fever, and joint pain.
- Treatment: Corticosteroids or Thalidomide (strictly controlled due to birth defects).
Pharmacist’s Note: Patients often think the treatment isn’t working when a reaction occurs. It is vital to explain that this is actually the immune system “waking up” and attacking the bacterial debris. Never stop MDT during a reaction unless instructed by a specialist.
Complications and Disability Prevention
The tragedy of leprosy lies not in the infection itself, but in the secondary disabilities caused by nerve damage.
- Anesthesia (Loss of Sensation): When a patient cannot feel pain, they do not notice cuts, burns, or blisters. An infected cut can lead to ulcers and bone infection (osteomyelitis).
- Self-Care Routine:
- Daily inspection of hands and feet for cuts.
- Soaking feet in water to hydrate dry skin (since sweat glands may stop working).
- Oiling the skin to trap moisture.
- Wearing protective footwear.
Global Statistics and Data Sources
According to the World Health Organization (WHO) Global Leprosy Update (2022 data):
- There were 174,059 new cases detected globally in 2022.
- India, Brazil, and Indonesia report the highest number of new cases.
- The number of new cases in children indicates active transmission in communities, highlighting the need for better contact tracing.
- More https://my.clevelandclinic.org/health/diseases/23043-leprosy-hansens-disease
- Medline https://medlineplus.gov/ency/article/001347.htm
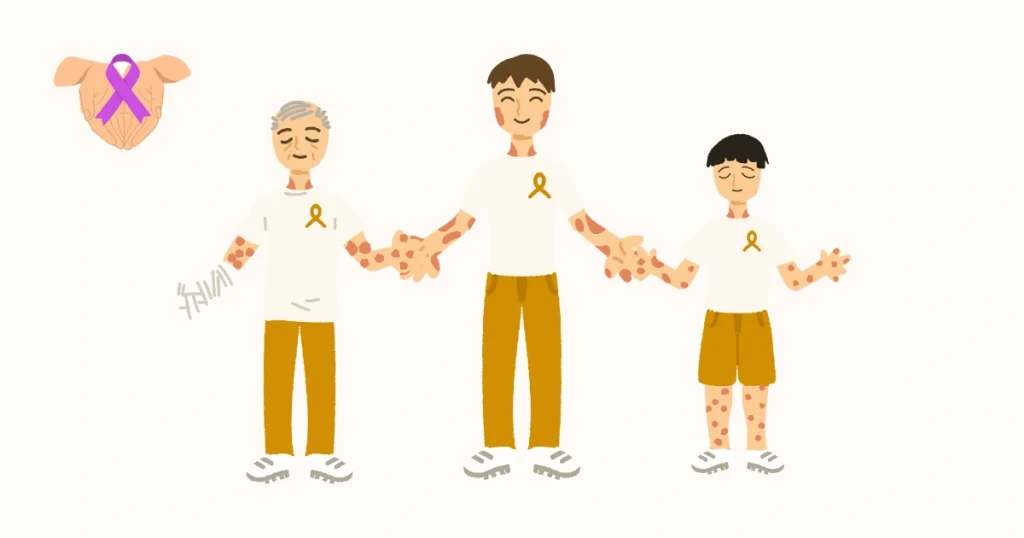
Breaking the Stigma
As healthcare providers, we fight two enemies: the bacterium and the stigma. Historical laws isolating patients in “leper colonies” are obsolete. Patients on MDT become non-infectious very quickly—often within 72 hours of starting Rifampicin.
There is no need for isolation. Patients can live with their families, go to work, and attend school while undergoing treatment. The physical deformities associated with leprosy are signs of untreated or late-treated disease, not active infection.
Conclusion
Leprosy is fully curable, and the medication is provided free of charge in most endemic countries through the WHO. If you notice a persistent skin patch that has lost sensation, or unexplained numbness in your extremities, seek medical advice immediately.
The journey from diagnosis to cure is well-charted. With strict adherence to the Multi-Drug Therapy regimen and proper self-care, patients can lead normal, healthy lives free from the burden of this ancient disease. DrugsArea
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult a physician or pharmacist for diagnosis and treatment.
FAQ about Leprosy (Hansen’s Disease), designed to provide clear, medically accurate, and stigma-busting information.
1. What is Leprosy (Hansen’s Disease) exactly?
Leprosy is a chronic infectious disease caused by a slow-growing bacteria called Mycobacterium leprae. It primarily affects the skin, the peripheral nerves (nerves outside the brain and spinal cord), the mucosa of the upper respiratory tract, and the eyes.
- Note: It is now preferably called Hansen’s Disease to reduce the historical stigma associated with the term “leprosy.”
2. Is Hansen’s Disease highly contagious?
No. This is one of the biggest myths about the disease.
- Transmission: It is hard to catch. It spreads through droplets from the nose and mouth during prolonged, close contact (over months) with someone who has untreated leprosy.
- Casual Contact: You cannot get it from casual contact like shaking hands, sitting next to someone on a bus, or sharing a meal.
- Natural Immunity: Remarkably, about 95% of all adults are naturally immune to the bacteria and will not get the disease even if exposed.
3. Is there a cure?
Yes, it is 100% curable.
Since 1981, the World Health Organization (WHO) has recommended Multidrug Therapy (MDT). MDT is a highly effective combination of antibiotics (typically dapsone, rifampicin, and clofazimine) that kills the bacteria.
- Treatment Duration: Treatment usually lasts between 6 to 12 months, depending on the severity.
- Availability: The medication is often provided free of charge by the WHO in endemic countries.
4. What are the early signs and symptoms?
Early detection is critical to preventing nerve damage.
- Skin: Pale or reddish patches of skin that may be numb (loss of feeling). This lack of sensation is a key differentiator from other rashes.
- Nerves: Numbness or tingling in the hands, feet, arms, or legs.
- Weakness: Muscle weakness or paralysis (e.g., difficulty gripping objects).
- Other: Painless wounds or burns on hands and feet (because pain receptors are damaged).
5. Is it true that body parts “fall off”?
No, this is a myth. The disease itself does not cause fingers or toes to drop off.
- The Reality: The bacteria attack the nerves, causing a loss of sensation. Because patients cannot feel pain, they may accidentally burn, cut, or injure their hands and feet repeatedly. These injuries can become infected, leading to tissue loss or the need for amputation if left untreated. This physical damage is secondary to the loss of feeling, not a direct effect of the bacteria “eating” the limbs.
6. Once treatment starts, is the person still infectious?
No.
Patients become non-infectious very quickly—often within 72 hours of starting the first dose of Multidrug Therapy.
- Isolation: There is absolutely no need for isolation or quarantine. Patients can continue to live with their families, go to work, and attend school while undergoing treatment.
7. What happens if the disease is left untreated?
If ignored, the bacteria can cause progressive and permanent damage, including:
- Paralysis: Crippling of hands and feet (e.g., “claw hand”).
- Blindness: Due to damage to the facial nerves that control blinking, leading to corneal drying and scarring.
- Disfigurement: Collapse of the nasal bridge or chronic non-healing ulcers on the soles of the feet.
8. Who is most at risk of getting it?
While anyone can technically get it, the risk is highest for:
- People living in endemic regions (currently, the highest rates are in India, Brazil, and Indonesia).
- Individuals living in prolonged close quarters with an untreated patient.
- Animal Vectors: In the southern United States, some armadillos carry the bacteria and can transmit it to humans, though the risk is generally low.
9. Why is there so much stigma surrounding the disease?
The stigma is largely historical, stemming from ancient times when the disease was incurable and disfiguring.
- “Curse” Myth: Many cultures viewed it as a curse or punishment for sin.
- Fear of Contagion: Before antibiotics, isolation (leper colonies) was the only management, reinforcing fear.
- Reality Today: Medical science has proven it is just a bacterial infection, like strep throat or tuberculosis, that is easily treatable.
10. Can I get tested if I think I was exposed?
There is no simple blood test that can easily diagnose Hansen’s disease in its early stages for everyone.
- Diagnosis: Doctors typically diagnose it by looking for the specific skin spots with sensory loss and may take a skin biopsy (removing a tiny piece of skin) to look for the bacteria under a microscope.
- Action: If you have a skin patch that doesn’t heal and has lost feeling, you should see a dermatologist or infectious disease specialist immediately.

